Introduction
Physiotherapy in Cambridge, Galt, and Preston for Ankle Issues
Welcome to The Cambridge Physiotherapy’s guide to psoriatic arthritis.
 Psoriasis is a disease that most people think of as primarily a skin disease because the condition causes a persistent rash in various areas of the body. Psoriatic arthritis is a type of joint disease that occurs in roughly seven percent of people who have psoriasis. Psoriatic arthritis affects people of all ages, but most get it between the ages of 30 and 50. Usually a patient has psoriasis (the skin rash) for many years before the arthritis develops, and usually the arthritis comes on slowly, however, this is not always the case. No matter what, patients with psoriatic arthritis must unfortunately manage both the outbreaks of itchy, scaly skin and the pain and stiffness of arthritis.
Psoriasis is a disease that most people think of as primarily a skin disease because the condition causes a persistent rash in various areas of the body. Psoriatic arthritis is a type of joint disease that occurs in roughly seven percent of people who have psoriasis. Psoriatic arthritis affects people of all ages, but most get it between the ages of 30 and 50. Usually a patient has psoriasis (the skin rash) for many years before the arthritis develops, and usually the arthritis comes on slowly, however, this is not always the case. No matter what, patients with psoriatic arthritis must unfortunately manage both the outbreaks of itchy, scaly skin and the pain and stiffness of arthritis.
This guide will help you understand:
- how psoriatic arthritis develops
- how doctors diagnose the condition
- what can be done for the problem
- what The Cambridge Physiotherapy’s approach to rehabilitation is
Anatomy
Where does psoriatic arthritis develop?
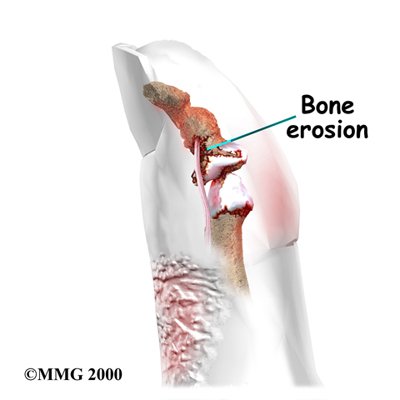
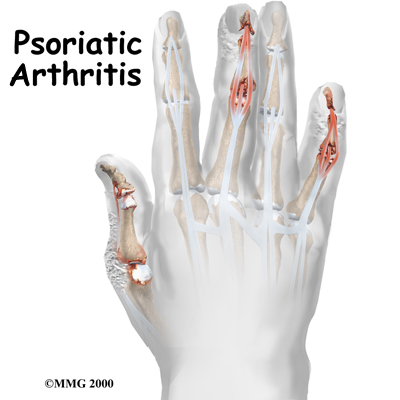
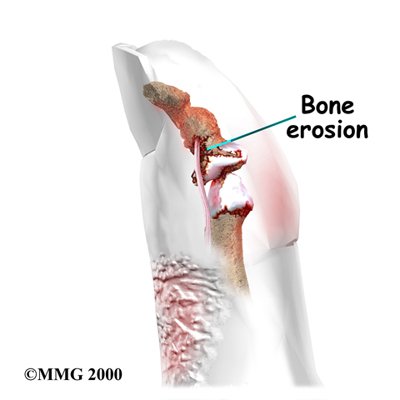
Psoriatic arthritis can affect any joint. Its symptoms often seem like the symptoms of rheumatoid arthritis (RA) or degenerative arthritis of the spine. X-rays can be used to show the difference between psoriatic arthritis and other diseases. In psoriatic arthritis, X-rays show a very distinctive type of bone destruction around the joints as well as certain patterns of swelling in the tissues surrounding the joints.
 Patients with psoriatic arthritis fall into three groups. The first group involves patients who have what is called asymmetric arthritis. This means that only a few joints are involved and that it does not occur in the same joints on both sides of the body. (For example, only one wrist and one foot are affected.)
Patients with psoriatic arthritis fall into three groups. The first group involves patients who have what is called asymmetric arthritis. This means that only a few joints are involved and that it does not occur in the same joints on both sides of the body. (For example, only one wrist and one foot are affected.)
An equal number of patients fall into the second group and suffer from symmetric polyarthritis. This means that arthritis occurs in several corresponding joints on both sides of the body. (For example, both elbows, both knees, and both hands are affected.) The polyarthritis type of psoriatic arthritis is much like RA.
A third group has mostly axial disease. This refers to arthritis of the spine, the sacroiliac joint (where the pelvis and bottom of the spine meet), or the hip and shoulder joints. Patients do not necessarily stay in the same category. Over time, the pattern may change. Doctors use these categories to better understand the disease and to follow the progression of the arthritis but the overall treatment is basically the same.
Causes
Why do I have this problem?
The exact cause of psoriatic arthritis is not known. Many factors seem to be involved in its development. Heredity plays a major role. People who are closely related to someone with psoriatic arthritis are 50 times more likely to develop the disease themselves. Recent studies have located genetic markers shared by most people who have the disease.
Sometimes injuries seem to set off psoriatic arthritis. Infections also contribute to the disease. It is known that strep infections in children can cause psoriasis. Some researchers think that the arthritis may be an immune system response to bacteria from the skin lesions.
Symptoms
What does psoriatic arthritis feel like?
All people who suffer from psoriatic arthritis have psoriasis (the skin rash). Some patients have very few areas of rash while other patients have psoriasis over a large portion of their bodies. The skin lesions of psoriasis are reddish, itchy, and have silvery scales. These areas can range in size from the size of a pencil dot to large areas the size of your palm. Psoriasis usually shows up on the elbows, knees, scalp, ears, and abdomen, but it can appear anywhere. In people with psoriatic arthritis, the psoriasis most often affects fingernails or toenails. The nails may have pits or ridges, or they may be discolored or appear to be separating from the skin.
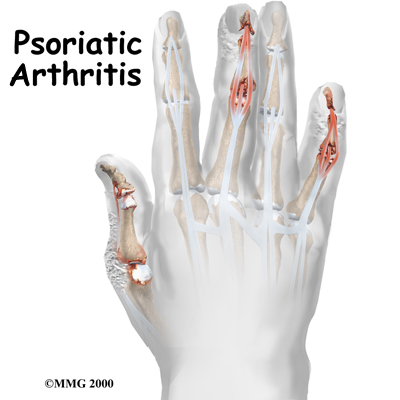
Psoriatic arthritis can affect any joint. Symptoms often seem like those of any other type of arthritis, such as joint swelling and pain. Some joint symptoms are unique to psoriatic arthritis:
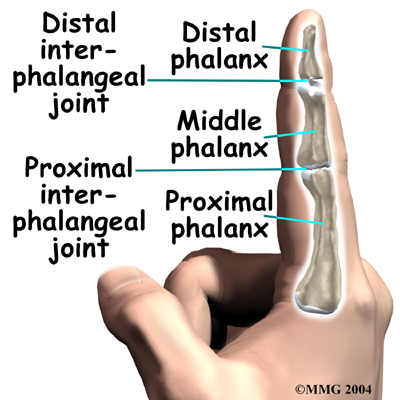
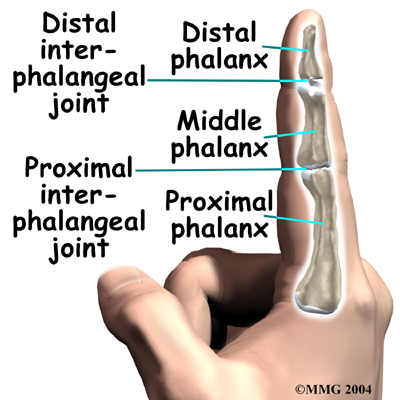
- The joints nearest to the fingernails and toenails are affected more. (These joints are called distal interphalangeal, or DIP joints.)
- The affected fingers and toes take on a "sausage-like" appearance.
- The bones themselves become inflamed (called dactylitis).
- The tendons and ligaments become inflamed where they attach to bones. (This is called enthesitis and is especially common in the heels.)
- Bony ankylosis of the hands and feet develops. (This means that the joints stiffen and become frozen in awkward positions.)
- The joints grow inflamed where the bottom of the spine meets the pelvis. (This is called sacroiliitis.) Patients often notice no symptoms, but the inflammation can be seen on X-rays.
- The vertebrae of the spine become inflamed. (This is called spondylitis.)
- The eyes become inflamed.
About five percent of patients with psoriatic arthritis will develop a form of arthritis called arthritis mutilans. This type of arthritis affects the small joints of the hands and feet. It is especially severe and destructive. The destruction caused by arthritis mutilans can result in deformity of the hands and fingers.
Rare symptoms include problems with the aortic heart valve, extra tissue formation in the lungs, and metabolic disorders that affect the tissues.
Diagnosis
How do health care professionals identify the condition?
A detailed medical history with questions about psoriasis in your family, will help your healthcare professional make a diagnosis. Patients with psoriasis may have other forms of arthritis, and the symptoms of psoriatic arthritis often look like other types of joint disease. This means that your doctor will probably do tests to rule out other diseases.
Blood studies will help rule out RA. (The RA test is usually not positive in patients with psoriatic arthritis.) Efforts are being made to find ways to identify psoriatic arthritis through a blood test. The presence of specific biologic elements called biomarkers (biologic evidence of disease) would make it possible to look for evidence of this disease before it progresses, or even before it starts. Psoriatic arthritis is common in people who test positive for HIV, the AIDS virus. As a precaution, your doctor may test your blood for HIV, especially if your symptoms are severe.
Physicians must also use other diagnostic tools such as X-rays, ultrasonography, and Magnetic Resonance Imaging (MRIs) in order to definitively diagnose psoriatic arthritis. Each one of these tests provides a little different information. For example, X-rays of affected joints will be studied both to rule out other diseases and to identify characteristics of psoriatic arthritis.
Ultrasonography, the use of sound waves to create a picture of what's going on inside, provides a better look at the whole package: bones, joints, and soft tissues. This diagnostic test is also noninvasive and does not expose the patient to any radiation. Ultrasound also has the ability to show small changes in the nails and early signs of inflammation in tendons and small joints.
MRIs can show bone marrow edema, tenosynovitis and early joint erosion. Tenosynovitis is the inflammation of the fluid-filled sheath (called the synovium) that surrounds a tendon. Unfortunately reliability is a problem with MRIs because what one examiner sees may not be the same as another observer. Changes in the small joints of the hands and feet don't show up well on MRIs like they do with ultrasonography.
One advantage MRIs do have over ultrasonography is the availability of whole body MRIs. By scanning the entire body, it is possible to identify areas of inflammation undetected by clinical examination.
Until blood studies are able to find biomarkers indicating the presence of psoriatic arthritis, physicians will have to continue to use a combination of different tests to diagnose the problem. The information these tests provide is important in determining treatment.
Treatment
What can be done for the condition?
Dealing with psoriatic arthritis involves treating both the skin lesions and the joint pain. Many lotions and creams are made for skin affected by psoriasis.
PUVA therapy, which stands for psoralen combined with ultraviolet A (UVA), may be helpful for the skin lesions. PUVA therapy uses topical cream medications that are rubbed on the skin lesions and affected joints. Following application of the cream, the skin area is placed under a lamp that emits a special ultraviolet light. The light triggers chemicals in the medication cream that treat the rash lesions and in some cases may also help the pain in the joints.
Treatment of arthritis symptoms depends on which joints are affected and the severity of the disease.
The first drugs most doctors prescribe are nonsteroidal anti-inflammatory drugs (NSAIDs). Aspirin and ibuprofen are NSAIDs, as are many prescription pain relievers. Other medications known as disease-modifying antirheumatic drugs (DMARDs) are used in patients with high levels of pain or particularly bad arthritis. These medications work in different ways to regulate the immune system and thereby control the arthritis.
One of the most commonly used disease-modifying medications for the treatment of psoriatic arthritis is methotrexate. DMARDs like methotrexate not only controls symptoms, they also slow the progression of disease. That's what makes them "disease-modifying". Methotrexate can control bad skin symptoms as well as help the arthritis symptoms. For some patients, it may be necessary to combine methotrexate with another drug (e.g., infliximab) to get the desired results (decreased joint pain, swelling, and stiffness).
Infliximab is a type of disease-modifying medication in a class called anti-tumor necrosis factor (TNF) agents. The anti-TNF agents are a special type of antibody referred to as human monoclonal antibodies. They specifically target (and inhibit) tumor necrosis factor. Tumor necrosis factor (TNF) promotes the inflammatory response, which in turn causes many of the clinical problems associated with autoimmune disorders such as rheumatoid arthritis.
Oral medications (pills taken by mouth) are under investigation and might be available in the future for the treatment psoriatic arthritis. These include ustekinumab, apremilast, and tofacitinib. Each of these medications works in a slightly different way to regulate the immune system.
Doctors will sometimes prescribe a combination of drugs. Cortisone injections into sore joints can also help relieve pain. Surgery may be called for in the rare cases of unmanageable pain or loss of joint function.
In addition to medicinal treatment your doctor will ask you to see a physiotherapist to maximize the strength and mobility of your joints.
Rehabilitation
Treatment for psoriatic arthritis at The Cambridge Physiotherapy can assist the management of your disease alongside the use of your prescribed medications. Physiotherapy cannot cure your disease, but it can assist in managing your pain and preventing a decline in your joints due to the disease process. Physiotherapy will focus on the effects of psoriatic arthritis on your joints rather than the skin lesions that are part of the disease.
During your first visit to The Cambridge Physiotherapy your physiotherapist will take a detailed history from you. They will want to know when the arthritis first started bothering you, which joints you have pain in, how often they bother you, the level of pain, and what sort of activities irritate or relieve your pain. They will also inquire about the associated skin lesions as well as any family history you may have of the disease, and any previous or current treatments you are undergoing, including which medications you are taking. Finally, they will ask about your work and recreational activities and will want to know if your arthritis limits you in any of these activities.
If your arthritis has affected any joints in your lower extremities your physiotherapist will want to watch the way you walk to see if your arthritis has affected your gait. They will also assess your overall posture and alignment to determine if you have developed any bad posturing habits or improper alignment due the disease. They will advise you on proper posturing and walking techniques and if needed, will discuss using a walking aid such as a cane/stick if they feel it is necessary to take some of the stress off of your joints.
Next your physiotherapist will assess and measure the range of motion in any joints that have been affected by the arthritis. Strength of the muscles surrounding these joints will also be determined. For any joints that have a decreased range of motion or are at risk of losing their range of motion, your therapist will prescribe range of motion exercises. Stretches will be prescribed for any muscles around the joints that are deemed to be tight and pulling adversely on the area. Strengthening exercises will be prescribed for any weak muscles or muscles that your therapist determines are at risk of losing strength over time due to the disease process.
Often doing exercises in a warm therapy pool can be easier on your joints and more comfortable so your therapist may encourage this for you. In addition, cardiovascular exercise can also be done more comfortably while in the pool (ie: water running, water aerobics, or swimming.) Doing a cardiovascular exercise of some sort is extremely important to managing your psoriatic arthritis as it keeps the body and joints limber and is excellent for your overall physical and mental well being. Stress can make your symptoms worse so cardiovascular exercise is an excellent method of helping to decrease your overall stress. If you are overweight, cardiovascular exercise is particularly important to assist you in weight reduction as the added weight on your joints can accelerate the wear and tear on them and increase any pain you may feel. If you are not interested in the pool or prefer exercise on the land you could use a stationary cycle, a stepper machine, an elliptical, or simply walk. Your therapist can help to design a cardiovascular program that suits your individual needs, and can advise on which type of exercise would be best for you.
In some cases of psoriatic arthritis, electrotherapy such as transcutaneous nerve stimulation (TENS) may be useful to decrease your joint pain. Your physiotherapist may also use hands on techniques such as massage for the muscles surrounding your joints, or mobilizations to encourage increased range of motion in your joints. Often the use of heat can be very soothing for your joints, so this may be used in conjunction with other therapy treatments. If you find the warmth soothing to your joints your therapist will encourage you to apply heat at home as well.
Unfortunately your psoriatic arthritis will not go away. However, there are many treatment options to help you manage this disease. Together with advice from your doctor, your physiotherapist, and any other healthcare professionals that are involved in your treatment you should be able to find a management program that will work for you.
Portions of this document copyright MMG, LLC.
The Cambridge Physiotherapy provides services for physiotherapy in Cambridge, Galt, and Preston.
 Psoriasis is a disease that most people think of as primarily a skin disease because the condition causes a persistent rash in various areas of the body. Psoriatic arthritis is a type of joint disease that occurs in roughly seven percent of people who have psoriasis. Psoriatic arthritis affects people of all ages, but most get it between the ages of 30 and 50. Usually a patient has psoriasis (the skin rash) for many years before the arthritis develops, and usually the arthritis comes on slowly, however, this is not always the case. No matter what, patients with psoriatic arthritis must unfortunately manage both the outbreaks of itchy, scaly skin and the pain and stiffness of arthritis.
Psoriasis is a disease that most people think of as primarily a skin disease because the condition causes a persistent rash in various areas of the body. Psoriatic arthritis is a type of joint disease that occurs in roughly seven percent of people who have psoriasis. Psoriatic arthritis affects people of all ages, but most get it between the ages of 30 and 50. Usually a patient has psoriasis (the skin rash) for many years before the arthritis develops, and usually the arthritis comes on slowly, however, this is not always the case. No matter what, patients with psoriatic arthritis must unfortunately manage both the outbreaks of itchy, scaly skin and the pain and stiffness of arthritis.








 Patients with psoriatic arthritis fall into three groups. The first group involves patients who have what is called asymmetric arthritis. This means that only a few joints are involved and that it does not occur in the same joints on both sides of the body. (For example, only one wrist and one foot are affected.)
Patients with psoriatic arthritis fall into three groups. The first group involves patients who have what is called asymmetric arthritis. This means that only a few joints are involved and that it does not occur in the same joints on both sides of the body. (For example, only one wrist and one foot are affected.)