Introduction
Physiotherapy in Cambridge, Galt, and Preston for Rheumatoid Arthritis
 Welcome to The Cambridge Physiotherapy’s guide to Rheumatoid arthritis (RA).
Welcome to The Cambridge Physiotherapy’s guide to Rheumatoid arthritis (RA).
RA is a chronic, or long-term, inflammatory form of arthritis. RA is considered an autoimmune disease, in which your immune system attacks the tissues of your own body. In RA, the immune system mostly attacks tissues in the joints, but it can also affect other organs of your body. In some people, RA seems to run its course and does not gradually get worse. In others, RA gets progressively worse and leads to the destruction of joints. RA can greatly affect your ability to move and do normal tasks. RA can appear at any age, but most patients are between the ages of 30 and 50. About two million Americans have RA, and most of them are women. RA can affect children and when it does, it is termed Juvenile RA. Juvenile RA will not be discussed in this patient guide.
This guide will help you understand:
- how RA develops
- how your health care professional will diagnose the condition
- what can be done for RA
- what The Cambridge Physiotherapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Arthritis|limit:15|heading:Hear from some of our patients who we treated for *Arthritis*#
Anatomy
How does RA develop?
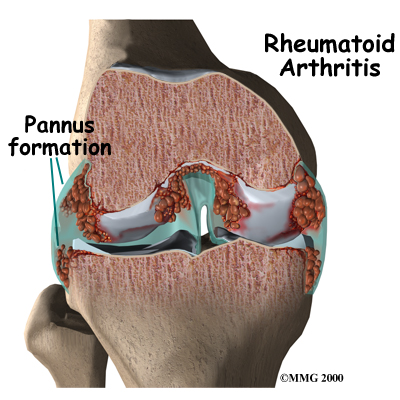
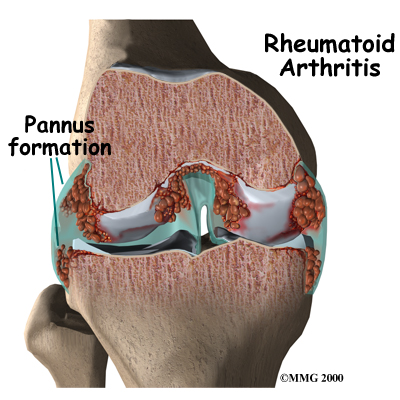
In RA, two processes are occurring in the joints. First, the immune system causes inflammation in the synovial membrane, called synovitis. The synovial membrane is the thin tissue that surrounds all joints. The synovitis is characterized by extra fluid, swelling, and warmth of the joint due to the increased blood flow.
The second process causing the problems in RA results from the ongoing or repetitive synovitis. The blood cells and the swollen membranes of the synovium release chemicals into the synovial fluid (the lubricating fluid of the joint) that can break down or damage the tissues of the joint. This breakdown can cause permanent damage to the cartilage, bones, ligaments, and tendons inside and around the joint. The structural damage usually happens in the first to third year of the disease. The synovitis can come and go, but the structural deterioration progresses and results in permanent damage. As a result, the joint becomes chronically painful and very difficult to move.
RA usually affects many joints on both sides of body (for example, both knees, both ankles, both wrists, and the same joints in both hands may be affected.) Research indicates that almost all the joints that will be affected long term show symptoms of RA in the first year of the disease. This means that each joint may continue to get worse, but you probably won't have many more joints that will develop the symptoms of RA.
Most RA patients also have inflammation in the tendons around the joint. (Tendons connect muscle to bone.) Nodules, or bumps, may form on the tendons, or the tendon sheath (the membrane that surrounds the tendon.)
Most people think of RA as an inflammatory disease of just the joints and related tissue, but it is actually a systemic disease meaning that it affects the whole body. In general, inflammation causes symptoms of swelling, redness, heat, and pain. RA can even show up in organs such as the heart, blood vessels, lungs, and eyes. Sometimes RA occurs in joints and other organs, and sometimes it occurs only in other organs. RA works somewhat differently outside the joints, but the underlying problem is still damage to the tissue and loss of function.
Rheumaotid factor (RF) is an antigen found in about 85 percent of RA patients. Not all patients with RA have RF in their blood. Some patients with RA do not have RF, and people with RF can have forms of arthritis that are not RA. Being RF positive, however, increases your likelihood that your organs will also be affected by RA.
Causes
Why do I have this problem?
No one knows exactly what causes RA. There are probably different causes in different people. Many doctors and researchers think that a virus or bacteria might cause RA. So far studies have not proven this. Researchers do know, however, that bacteria can cause swelling in the synovial membrane.
Heredity, or your genes, play a part in RA. The disease tends to run in families. If a close relative has RA, you are 16 times more likely to develop the disease yourself.
Symptoms
What does RA feel like?
The primary symptom of RA is pain in symmetrical joints (i.e.: both elbows, both knees, and so on). In rare cases the pain is only in one joint. Most often the pain develops over several weeks but the pain can come on suddenly. As the pain spreads to other joints, it usually then becomes more symmetrical. The pain is directly related to the amount of swelling in the synovial membranes. When the swelling is at its worst, your joints themselves will feel warm and swollen. The pain can come and go with the swelling.
RA patients also describe severe morning stiffness that can last up to two hours. The stiffness can be so bad that it makes it hard to get dressed, make breakfast, or even get out of bed. This stiffness also corresponds to the synovitis. When the synovitis goes away for a time, so does the stiffness.
About half of RA patients have rheumatoid nodules. As described above, the nodules are hard knots, from the size of a pea to the size of a golf ball, that grow on the sheath of tendons or under the skin. They are usually found on the outside of the elbow, the Achilles tendon on your heel, the underside of your fingers, the lower abdomen, and certain toe joints. The nodules don't usually hurt and over time they tend to shrink or disappear.
Due to RA being a systemic disease, most patients feel tired and weak during flare-ups. About 50 percent of RA patients have systemic inflammation during joint outbreaks of RA.
Conjunctivitis, or inflammation of the eye, is a common symptom of RA. It may be related to a disease of the eye called Sjogren's syndrome, which often occurs along with RA. The main symptom is eye dryness, but patients often can't even feel it.
When RA affects the lungs it can cause an inflammation of the membrane that surrounds the lungs (the pleura.) This inflammation is called pleurisy and results in pain, problems breathing deeply, and sometimes coughing.
RA commonly affects the nervous system, but the symptoms from damage to the nervous system can be hard to distinguish from other symptoms of RA. Damage to the joints in the cervical spine (the neck) can eventually lead to weakness and instability between the cervical vertebrae. This damage can cause problems with the spinal cord as it travels through the neck and in turn, spinal cord symptoms can result.
Common symptoms of affected areas include the following:
- Cervical spine (the neck): Symptoms include neck stiffness, weakness, and loss of motion. Ligaments are often inflamed, and there may be problems with the spinal cord or nervous system as explained above. Neck pain alone tends to get better, even when the joints are damaged. Damage to the nervous system, however, does not usually improve.
- Shoulders: The main symptom is loss of motion. Your body's unconscious reaction to shoulder pain is simply to not use your shoulders. Since daily life doesn't require large shoulder ranges of motion, frozen shoulder syndrome, in which the shoulder joint’s range or motion becomes severely limited, can set in quickly.
- Hands and wrists: Almost everyone with RA has affected wrists and the joints in the middle of your hand and the middle joints of your fingers. The knuckles at the ends of your fingers usually are not. RA can cause joint deformities that freeze your fingers in unusual positions. Rheumatoid nodules and tendon inflammation can make it hard to bend the fingers. Nodules can cause a locking and catching action as your fingers bend.
- Knees: Swelling in the knees is common and can be easily seen. A fluid-filled lump called a Baker's cyst often appears behind the knee. It can burst and leak fluid into the calf.
- Feet and ankles: RA commonly affects the joints in the middle of the toes and the ankle joints. The deformities and pain in the toes can cause problems with walking. The sole of the foot can feel tingly or numb.
The progression of RA is hard to predict. The swelling of RA ‘flares up’ and dies down such that there may be times when there is not much pain at all. At other times, however, flare-ups cause significant pain. Milder forms of the disease often don't require much treatment. Even milder forms of RA may even go undiagnosed.
Diagnosis
How do health care professionals diagnose RA?
Diagnosis in its earliest form begins with a complete history and physical examination. When you visit your physiotherapist at The Cambridge Physiotherapy they will ask questions about when and how your pain began, what joints are involved, and what activities aggravate or relieve your pain. It is best if you can be very specific about where your pain is and when precisely it started. We may also ask about any previous injuries you may have had to your joints, as well as overall general health questions and questions about any family history of disease. The history is an extremely important part of any examination and may already lead your physiotherapist to the suspicion of RA.
Next your physiotherapist will do a physical examination of your joints. First they will simply look and feel your joints for any signs of swelling which may include redness, increase in size, warmth, or possible abnormalities in the joint position or abnormalities such as nodules. We will always compare both sides of your body for differences or similarities and will often check many joints even if they do not feel painful to you.
Next your physiotherapist will ask you to actively move your affected joints to assess your willingness and ability to move and also to determine if there is a range of motion deficit. Your physiotherapist may also ask you to relax your muscles while they passively move your joints to further assess the range of motion. While your joints are moving we will also be assessing for crepitus, which is a high-pitched screech or grinding that you can feel or hear in the joint when bone rubs directly on bone.
This sound can indicate that inflammation in the joint has worn down the tissue inside such that the ends of the joints are rubbing on each other. Lastly, we will also check for any signs of damage or looseness in the joints by stressing the ligaments (the tissues that attach bone to bone.)
If your physiotherapist deducts from the history and physical examination that your problem is potentially due to RA, we will refer you on to your doctor for further examination and investigations.
Physician’s Review
No single test can confirm a diagnosis of RA. Many findings over a period of time lead to the diagnosis. Early on, many characteristics of RA haven't developed yet, such as the pattern of joints that are affected, X-ray findings, and blood test changes. RA in its early stages can look a lot like other orthopaedic problems or other forms of arthritis, such as lupus, psoriatic arthritis, and diseases of the spine or simple orthopaedic problems. Your doctor will need to consider each of these diagnoses and perhaps do tests to rule them out.
To confirm the presence of inflammation in the synovial membranes, which occurs in all patients with RA, your doctor can do a count of the white blood cells (WBC) in your synovial fluid. This test involves inserting a thin needle into your joint and drawing out a small amount of the fluid for testing. The fluid can also be tested for other things. The WBC alone, however, doesn't prove that you have RA. Synovitis of the joints can occur even if you don’t have RA therefore your doctor will need to rule out other causes of synovitis.
Your doctor will also ask you to undergo a blood test. As mentioned previously, RF, or rheumatoid factor, is found in the blood of about 85 percent of RA patients. This test alone can't confirm RA either. Some patients with RA do not have RF, and people with RF can have other forms of arthritis.
Another test your doctor can determine from your blood is the erythrocyte sedimentation rate (ESR, or sed rate), which measures how fast red blood cells settle in the test tube. Red blood cells that settle faster than normal indicate inflammation in the body. The ESR varies greatly between people. It is even possible for a patient with RA to have a normal ESR. The ESR may be more useful in monitoring the progress of RA than in diagnosing it. A higher ESR, however, usually means that the inflammation is more severe.
The C-reactive protein test can also monitor inflammation. It is a newer test that may be more accurate than the ESR. This test measures the amount of a certain protein that is produced by the body due to inflammation. When inflammation is very active the amount of C-reactive protein is high, and when inflammation is brought under control the level of protein decreases.
At some point your doctor will probably ask you to get X-rays of your affected joints and organs. X-rays and other imaging techniques can show damage to the cartilage and bone as well as swelling in the soft tissues of the joint.
If you have rheumatoid nodules your doctor may want to take a biopsy of them. During the biopsy a small amount of the nodule is removed and examined in a laboratory.
Treatment
What can be done for the condition?
Doctors have learned a lot about RA in recent years, but they still don't know much more about how to truly cure the disease. They do have many medical strategies for treating the symptoms of RA. This treatment includes both medication as well as physical rehabilitation. If you start treatment within a few months after your symptoms appear, you will probably do better in the long-term. Early detection and treatment can help avoid the worst joint damage. Sudden remission does occur, but it's unclear how often, and it appears to be more likely within the first two years of the disease. Patients, who develop RA at a young age, are RF positive, have close relatives with RA, and have RA nodules tend to have a more difficult time managing the disease.
Medication
Your doctor will prescribe one or more medications.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, can help decrease the pain and swelling.
Corticosteroids taken by mouth can also help with inflammation but should not be used long term if at all possible due to the other problems they can cause in your body. Corticosteroid injections into the affected joints can ease the swelling and give immediate, short-term relief. Due to eye inflammation being so common with RA and difficult to diagnose, your doctor may also prescribe eye medications, even if you have no eye symptoms. Prophylactic eye drops can help prevent symptoms from developing or becoming severe when they start.
Disease-modifying antirheumatic drugs (DMARDs) are important in treating RA. It is not certain exactly how DMARDs actually slow or prevent the structural damage from RA however, tests have shown all DMARDs to be effective.
Unfortunately, DMARDs can be very hard on the body and can interact with other drugs. Often more than one DMARD is taken at the same time and it is not always easy to find the best combination of drugs that work for each individual. Common DMARDs frequently prescribed are:
Hydroxychloroquine: A relatively nontoxic drug that was made to treat malaria. It can be safely used with other DMARDs. It is most useful in early, mild RA. Regular eye check-ups should be conducted while taking this drug.
Sulfasalazine: Much like hydroxychloroquine. This drug requires regular blood monitoring.
Gold salts: Can cause short-term remissions. Over the long-term, however, the RA does progress.
Blood and urine monitoring is required.
Methotrexate: Can help manage RA, but it is unclear how much it actually changes the course of the disease. Methotrexate can be very useful over the long-term, but there are problems with flare-ups when patients stop taking it.
Azathioprine: Used with moderate and severe RA.
Penicillamine: Only used in patients who have systemic disease that doesn't respond well to other medications.
Cyclosporine: Expensive and hard on the kidneys, so it is most often used in severe RA.
Cyclophosphamide: Very effective but very toxic, so it is only used in specific cases.
Certain antibiotics are somewhat effective in mild cases.
Biologic response modifiers (BRMs) are among the newest drugs used to treat rheumatoid arthritis.
They are genetically engineered proteins derived from human genes and are designed to inhibit specific components of the immune system that play pivotal roles in fueling inflammation, which is a central feature of rheumatoid arthritis.These agents inhibit key factors responsible for inflammatory responses in the immune system. Common biologics frequently prescribed are abatacept (Orencia), etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), and anakinra (Kineret).
Abatacept inhibits T-cell activation. T-cells are types of white blood cells that cause swelling and joint damage in patients with RA.
Etanercept, infliximab and adalimumab are tumor necrosis factor (TNF) antagonists. TNF is responsible for both joint inflammation and other systemic inflammatory responses in RA patients
Anakinra inhibits interleukin-1 (IL-1). Interleukin-1 in RA amplifies and perpetuates the inflammatory process related to the lining of the joints. This leads to the destruction of the cartilage and bones inside the joints.
Biologics are used to treat moderate to severe rheumatoid arthritis that has not responded adequately to other treatments. They differ significantly from traditional drugs used to treat rheumatoid arthritis in that they target specific components of the immune system instead of broadly affecting many areas of the immune system. Biologics may be used alone but are commonly given along with other rheumatoid arthritis medications. They have been shown to help slow progression of rheumatoid arthritis when all other treatments have failed to do so.
Abatacept (Orencia): Abatacept is given intravenously (IV) as an infusion over 30 minutes. During the first month, it is given every 2 weeks, then every 4 weeks thereafter. It may be used alone or with DMARDs.
Etanercept (Enbrel): Etanercept is taken as an injection once or twice a week. It may be used alone or with concomitant therapy such as methotrexate.
Infliximab (Remicade): Infliximab is given as a 2-hour intravenous infusion in a doctor’s office. Initially, 3 doses are given within a 6-week period; thereafter, a single dose is given every 8 weeks to maintain the drug’s effect. The interval between doses is shortened if the 8-week regimen fails to control symptoms. It is most often used with concomitant methotrexate.
Adalimumab (HUMIRA): Adalimumab is given as an injection every other week (or sometimes weekly). It is most often used with concomitant methotrexate.
Rehabilitation
Although there is no cure for RA, physiotherapy can greatly assist with both the flare-ups as well as the potential long-term joint problems that can occur as a result of the disease. The main goals of our treatment at The Cambridge Physiotherapy for RA are to relieve symptoms, preserve the function of your joints, prevent structural damage or deformity, and to assist you with maintaining a normal lifestyle.
The Cambridge Physiotherapy provides services for physiotherapy in Cambridge, Galt, and Preston.
RA is a frustrating and complex disease. At The Cambridge Physiotherapy we believe that the more you understand about the disease, the more effective our treatment will be. For this reason, education is an important part of our treatment for RA. By understanding the disease, you will also be better able to assist us in treating your own symptoms and preventing or managing flare-ups. Liaising with others who also have RA can be very insightful so we will assist in directing you to support groups or organizations that focus on living with RA.
As mentioned previously, the synovitis of the joints causes pain and over time can cause structural damage and deformities of the joints. During flare-ups the synovitis is actively occurring and is the source of pain. Our treatment at The Cambridge Physiotherapy will therefore firstly focus on decreasing your pain. Modalities such as heat or cold may be useful as well as other modalities such as transcutaneaous nerve stimulators (TENS.) These TENS machines assist with pain by delivering electrical currents through the painful area and work essentially to override the pain sensations. Your physiotherapist may also suggest that you use hydrotherapy to ease the pain. During hydrotherapy your whole body, or just the affected joints, are immersed in warm water while gentle movements are performed. In many cases, this can significantly reduce the pain associated with an RA flare-up. Massage can also be very helpful to assist with flare-ups although not all patients with RA enjoy their painful joints being massaged, and this will be entirely respected. Sometimes with RA the most effective treatment during a flare-up is simply to rest the joint. Each joint has a natural resting position where the least amount of stress is placed on the tissues of the joint and therefore causes the least amount of pain. Your physiotherapist at The Cambridge Physiotherapy can advise you on the most effective resting position for any of your RA affected joints and can also advise you on when it is appropriate to begin exercise again after the rest period.
In addition to our physiotherapy treatment the medication that your doctor has prescribed will be especially important during flare-ups. Your physiotherapist at The Cambridge Physiotherapy may liaise closely with your doctor while treating you to ensure that all treatments are coinciding to most effectively relieve your pain. By limiting the length and intensity of the flare-ups, the synovitis has less time to cause structural damage to the joints and therefore less chance of causing a long-term deformity.
The next part of our treatment at The Cambridge Physiotherapy will focus on preventing any deficits or deterioration in range of motion of your affected joints. Your physiotherapist may assist in stretching your muscles while at the clinic and, if necessary, may ‘mobilize’ the joint. This hands-on technique encourages joints to move gradually into their normal range of motion and may also assist with pain relief. We will also prescribe a series of stretching exercises that we will encourage you to do as part of a home exercise program. The daily stretches and range of motion exercises done at home are often the most important part of treating RA as they work to both prevent and stop the progression of long-term deformities in the joint. If your joints have already developed some deformity then we will be particularly specific in teaching you range of motion exercises that take into consideration the abnormal position of the joint. Standard stretching exercises may cause deformities to progress if not adjusted to this consideration. Your physiotherapist at The Cambridge Physiotherapy will tailor a stretching program specifically for you.
Joints where deformity is likely to occur or that already show some deformation may require bracing or splinting to prevent further decline. Simple braces may be constructed by your physiotherapist at The Cambridge Physiotherapy but for more complex braces we will refer you to an occupational therapist, orthotist, or chiropodist to ensure a proper individualized brace or orthotic is constructed. Occupational therapists can also provide you with assistive devices, if needed, which make using a joint affected by RA easier and less painful. This in turns prevents the deterioration of the joint.
The muscles surrounding the affected RA joints can lose strength. The strength loss occurs both due to decreased use of the joints when they are painful, and also as a result of the altered pulling on the muscles when there are joint deformities. Similarly to the range of motion deficits, strength deficits will also be addressed during our treatment. Again, your physiotherapist at The Cambridge Physiotherapy will prescribe a series of strengthening exercises that we will encourage you to do as part of a home exercise program. These exercises will also be specifically tailored by our physiotherapist to suit the needs of your affected joints.
Maintaining coordination of your RA joints is also an important part of maintaining normal function. Pain, inflammation, and joint deformity can all affect how well a joint works during functional activities such as grasping items or walking. In addition to the range of motion and strengthening exercises prescribed your physiotherapist at The Cambridge Physiotherapy will encourage coordination and proprioception exercises to ensure the joints do not lose normal function.
As a final component of our treatment, your physiotherapist will discuss the benefits of some gentle aerobic exercise. Aerobic exercise such as swimming, walking or cycling can improve muscle endurance, aerobic capacity and improve your general well-being so is highly encouraged as part of an overall treatment plan for patients suffering with RA. Obviously, during times of flare-ups, aerobic exercise may not be possible, however when able, you should work to include it.
Surgery
At least half of RA patients don't get effective relief from treatment and eventually need surgery on the affected joints. Surgery, including total joint replacement, can be a very effective way to help you overcome the pain and loss of movement of RA.
For most patients, RA is a disease that comes and goes throughout their lives but it doesn't have to be crippling. With the help of health care professionals such as your doctor and physiotherapist, you should be able to find treatment that works for you and allows you to maintain a normal lifestyle.
Portions of this document copyright MMG, LLC.
 Welcome to The Cambridge Physiotherapy’s guide to Rheumatoid arthritis (RA).
Welcome to The Cambridge Physiotherapy’s guide to Rheumatoid arthritis (RA).









