Introduction
Physiotherapy in Cambridge, Galt, and Preston for Foot Conditions
Welcome to The Cambridge Physiotherapy's guide to Achilles Tendon Problems.

Problems that affect the Achilles tendon include tendocalcaneal bursitis, tendonitis/paratendonitis, tendinopathy/tendonosis, and Achilles tendon ruptures. Each of these conditions will be described and explained. These problems often affect athletes, especially runners, basketball players, and anyone engaged in jumping sports. They are also common, however, among both active and sedentary (inactive) middle-aged adults. Severe cases may result in a rupture of the Achilles tendon.
This guide will help you understand:
- where the Achilles tendon is located
- what kinds of Achilles tendon problems there are
- how an injured Achilles tendon causes problems
- how health care professionals diagnose the condition
- what treatment options are available
- The Cambridge Physiotherapy’s approach to rehabilitation
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
Anatomy
 Where is the Achilles tendon, and what does it do?
Where is the Achilles tendon, and what does it do?
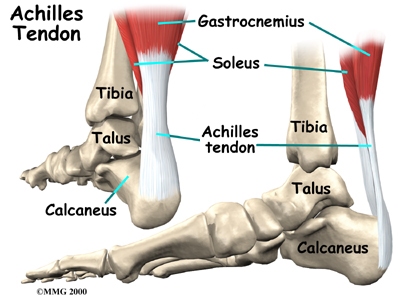
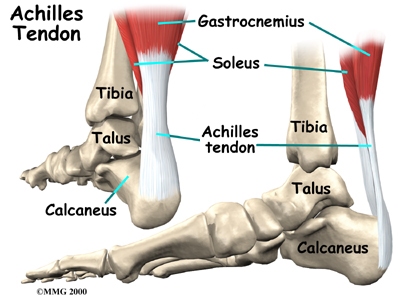
The Achilles tendon is a strong, fibrous band that connects the calf muscle to the heel. The calf is actually formed by two muscles, the underlying soleus and the thick outer gastrocnemius. Together, they form the gastroc-soleus muscle group. The insertion of the gastroc-soleus group into the heel is called the enthesis.
Foot Anatomy Ligaments & Tendons
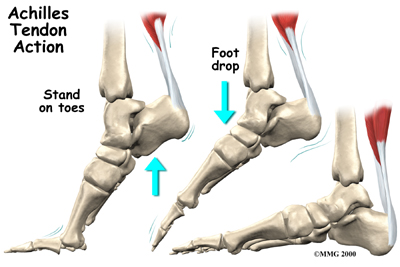
When muscles of the calf contract, they pull on the Achilles tendon, causing your foot to point down and helping you rise up onto your toes. This powerful muscle group is especially active when you sprint, jump, or climb but is also active during every regular step you take. Several different problems can occur that affect the Achilles tendon, some rather minor and some quite severe.
Tendocalcaneal Bursitis
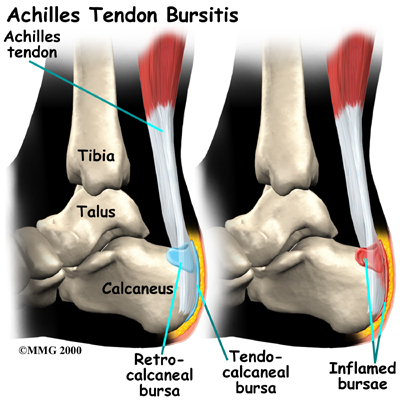
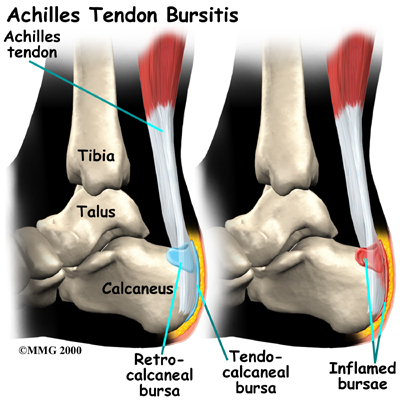
A bursa is a fluid-filled sac designed to limit friction between rubbing body parts. These sacs, or bursae, are found in many places in the body. When a bursa becomes inflamed, the condition is called bursitis. Tendocalcaneal bursitis is an inflammation in the bursa behind the heel bone. This bursa normally limits friction when the thick fibrous Achilles tendon that runs down the back of the calf glides up and down behind the heel. With increased or repetitive activity that causes increased friction, bursitis in this area can develop.
Achilles Tendonitis/Paratendonitis
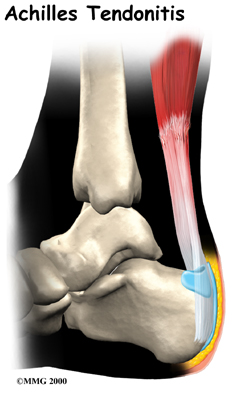
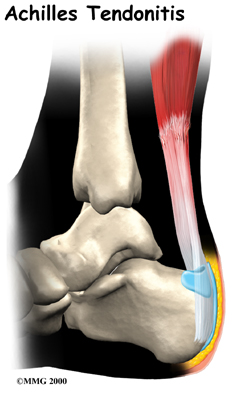 A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
The use of the term tendonitis to describe the common Achilles tendon injury has been disputed in recent years due to the fact that the suffix ‘itis’, in medical terminology, denotes the process of inflammation occurring. Studies have actually shown that in cases of chronic Achilles pain, there are no acute signs of inflammation so it is theoretically incorrect to use the ‘itis’ suffix to describe this injury. The common terminology of tendonitis generally refers to two subsets of separate injuries: paratendonitis, and tendonosis.
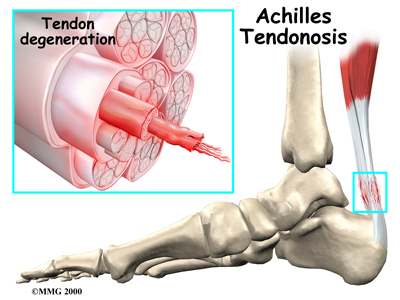
Achilles Tendonosis/Tendinopathy
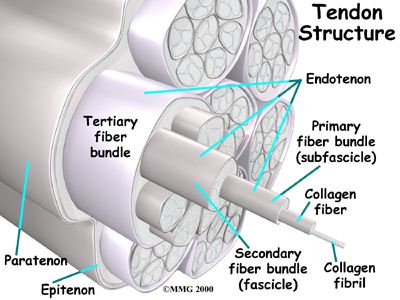
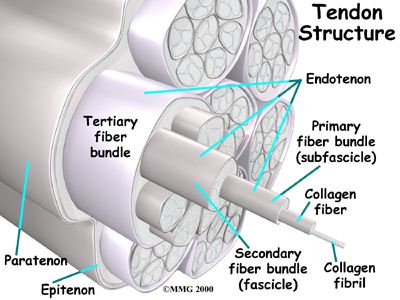
Chronic overuse or long term inflammation may contribute to changes in the Achilles tendon, leading to degeneration and thickening of the tendon. As mentioned above, studies show that although inflammation may have contributed to the initial changes in the tendon, there is no acute sign of inflammation in chronically painful tendons. Most experts now refer to this chronic condition as tendonosis or tendinopathy instead of the acute diagnosis of paratendonitis or tendonitis. Acute inflammation, however, is not a precursor to the development of tendonosis. The degeneration and thickening of the achilles tendon that is the hallmark of a tendonosis diagnosis can also develop over time simply from general wear and tear. Tendons are made up of strands of a material called collagen. (Think of a tendon as similar to a nylon rope and the strands of collagen as the individual nylon strands.) Degeneration in a tendon usually shows up as a loss of the normal arrangement of the fibers of the tendon. Some fibers even break (microtears,) and the tendon loses overall strength.
In these situations the body tries to naturally heal the tendon and this causes the tendon to become thickened as scar tissue and fatty tissue tries to fill in the deficits in the tissue. This process can continue to the extent that a nodule made up of scar tissue forms within the tendon. Tendonosis or tendinopathy is essentially failed healing. It is the accumulation of microscopic injuries over time that do not heal, and then lead to a chronically degenerated tendon. The weakened, degenerative tendon sets the stage for the possibility of actual rupture of the Achilles tendon.
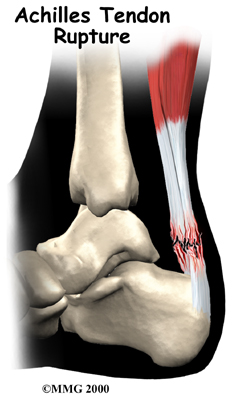
Achilles Tendon Rupture
In severe cases, the force of a violent strain may even rupture the Achilles tendon. The classic example is a middle-aged tennis player or weekend warrior who places too much stress on the tendon and experiences a tearing of the tendon. In some instances, the rupture may be preceded by a period of Achilles paratendonitis, or a tendonosis, which renders the tendon weaker than normal.
Related Document: The Cambridge Physiotherapy's Patient's Guide to Foot Anatomy
Causes
How do these problems develop?
 It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.
It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.
 Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.
Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.
Advancing age can also be a risk in the development of Achilles tendon problems. As we age, our tendons can degenerate. Degeneration means that wear and tear occurs in the tendon over time due simply to repetitive use, and this leads to a situation where the tendon is weaker than normal. There is also some thought that as we age we produce less of the resilient type of tissue in the tendons (called elastin) than when we are younger. The decreased amount of elastin then exposes the tendon to an increased risk of microtears and trauma.
Symptoms
What do these conditions feel like?
Tendocalcaneal bursitis usually begins with pain and irritation at the back of the heel. There may be visible redness and swelling in the area. The back of your shoe may further irritate the condition, making it difficult to tolerate shoe wear.
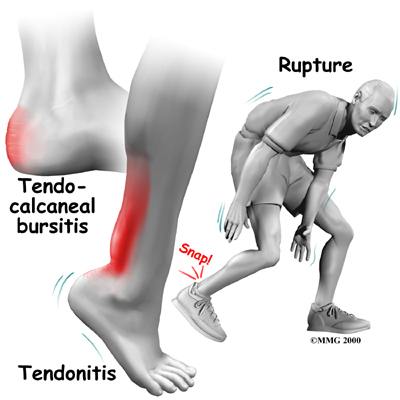
Achilles paratendonitis usually occurs a bit further up the leg, just above the heel bone itself. The Achilles tendon in this area may be noticeably thickened and tender to the touch. Pain is present with walking, especially when pushing off on the toes. You may also hear or feel what is called crepitus. Crepitus is a grating, crackling or popping sound and/or sensation that is experienced under the skin. Crepitus is not normal and is caused by the rubbing of structures upon each other; in regards to the Achilles tendon, this can be an inflamed paratenon on the Achilles tendon itself.
An Achilles tendon rupture is usually an unmistakable event although sometimes this injury does get initially misdiagnosed. The patient and even some bystanders may report actually hearing the snap of an Achilles tendon rupture, and the victim of a rupture usually describes a sensation similar to being violently kicked in the calf.
Following a full rupture the calf may swell, and the patient is usually unable to rise on their toes.
Diagnosis
Diagnosis begins with a complete history and physical examination. Your physiotherapist at The Cambridge Physiotherapy will ask questions about where precisely the pain around the Achilles is, when the pain began, what you were doing when the pain started, and what movements aggravate or ease the pain. As mentioned above, factors such as training history as well as type of footwear are important for us to inquire about. The history alone will often lead your physiotherapist to the diagnosis regarding your injury.
Next your physiotherapist will do a physical examination of the Achilles tendon, ankle and entire lower extremities. They will palpate, (touch) around the ankle and calf muscles and particularly along the Achilles tendon to determine the exact location of pain. Your physiotherapist will assess your alignment, flexibility and joint laxity in your ankle and lower extremity. If you are able they will want to look at your foot position, how you stand, walk, squat, run, or jump. Your physiotherapist will also check the strength and lengths of the muscles directly affecting the Achilles such as the calves and hamstrings and may also check other muscles such as the quadriceps, hip flexors and buttocks muscles. All of these muscles, if weak or tight, can contribute to the forces applied to the Achilles and contribute to the development of an Achilles problem. Pain is usually felt when your physiotherapist asks you to rise up on your toes. If you are unable to do this and your history is that of a sudden onset of Achilles pain, your physiotherapist will suspect a rupture of the tendon. In this case, squeezing of the calf muscle (Thompson Test) will be performed to see if a contraction of the calf causes the normally attached Achilles tendon to point the foot. If this does not occur, an Achilles tendon rupture is likely. The position of the relaxed foot when you are lying on your stomach is also important in determining a possible rupture. Instead of the natural slight pointing of the foot that occurs from the tension of the Achilles tendon, the foot hangs at nearly a 90-degree angle to the leg when there has been a rupture of the tendon. Close palpation of the tendon will often reveal a gap in the area of the two ends of the ruptured tendon if there is not too much swelling. If your physiotherapist suspects a ruptured Achilles tendon, we will liaise with your doctor regarding investigations to confirm this diagnosis. Appropriate immediate action regarding management of a ruptured tendon needs to be decided upon.
The Cambridge Physiotherapy provides services for physiotherapy in Cambridge, Galt, and Preston.
Physician’s Review
When an Achilles tendon rupture is suspected, a magnetic resonance imaging (MRI) scan or ultrasound may be necessary to confirm the diagnosis. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. The MRI creates images that look like slices and shows the tendons and ligaments very clearly. A basic MRI does not require any needles or special dye and is painless.
An ultrasound uses high-frequency sound waves to create an image of the body's organs and structures. The image can show if an Achilles tendon has partially or completely torn. By repeating this test over time it can be easily be determined if a tear has gotten worse.
By using the MRI and ultrasound tests, doctors can determine if surgery is needed. For example, a small tear may recover well with only physiotherapy treatment and may not require surgery.
Treatment
What treatment options are available?
Nonsurgical Treatment
In the past, nonsurgical treatment for injuries related to an Achilles tendon irritation started with a combination of rest, ice, and anti-inflammatory medications such as aspirin or ibuprofen, as well as physiotherapy.
Since it is now recognized that many tendon problems occur without inflammation, the use of anti-inflammatories and ice have come under question. Even in the case of true inflammation, the overuse of these modalities may prevent the normal inflammatory process from occurring and initiating the healing process. Preventing inflammation that is needed to clean up cellular debris in the injured area may lead to delayed or incomplete healing. The result may be future chronic problems of tendonosis/tendinopathy.
Many experts suggest when there is any doubt about inflammation; treatment should proceed as if there are no inflammatory cells present. This approach focuses on pain relief and restoring proper motion and biomechanics so you can return to your usual activities. In the case of true inflammation occurring, modalities to combat this are useful at the appropriate stage of rehabilitation. Cortisone injections to the tendon are still used if one is confident that excessive inflammation is present, however, they continue to be used cautiously as the tendon itself is known to weaken post injection.
Rehabilitation
What can I expect following treatment?
Nonsurgical Rehabilitation
Tendocalcaneal Bursitis/Paratendonitis
When you begin physiotherapy at The Cambridge Physiotherapy the type of treatment you will receive will depend on the particular problem you have present.
If there is a true inflammatory process present with your injury (i.e.: tendocalcaneal bursitis or paratendonitis) your initial treatment at The Cambridge Physiotherapy will aim to decrease excessive inflammation and pain. Our physiotherapists can assess when anti-inflammatory treatment is necessary and for how long this treatment should continue. Simply icing your Achilles can often relieve a lot of the acute pain. Your physiotherapist may also use electrical modalities such as ultrasound or interferential current to help decrease the pain and inflammation. Massage for the calf may also be helpful. In addition, a heel lift placed in your shoe can help take the tension off of a painful tendon. In order to not affect alignment, a lift is also placed in the other shoe. Some taping or strapping techniques we use at The Cambridge Physiotherapy can also be useful to decrease the pain caused by an Achilles tendon injury and allow healing to occur. Limiting, but not eliminating, inflammation is the goal. If inflammation is present, the injury should respond quite quickly to any anti-inflammatory treatments used.
Once the initial pain and inflammation has calmed down, your physiotherapist in Cambridge, Galt, and Preston will focus on improving the flexibility, strength, and alignment around the ankle joint and entire lower extremity. Static stretches for the calf will be prescribed by your physiotherapist early on in your treatment to improve flexibility and put gentle stress on the healing tissues which encourages them to properly align. Gentle stretching can also help with relieving pain. As mentioned above, any tightness in the muscles or tissues in the lower extremity can change the alignment and force put through the Achilles tendon therefore your physiotherapist will prescribe stretches for any of the muscles in the lower extremity that have been determined to be affecting your alignment. This may include stretches for the back or your thighs (hamstrings) or even your hips. Dynamic stretching (rapid motions that stretch the tissues quickly) will also be taught and will be incorporated into your rehabilitation exercise routine as part of your warm-up once you return to doing more aggressive physical activity. Dynamic stretches are used to prepare the tissues for activity whereas static stretches focus more on gaining flexibility.
Strength imbalances will also affect the alignment around the ankle and can cause muscles to tighten. Your physiotherapist will determine which muscles in your individual case require increased strengthening. Appropriate strength in areas above the ankle, in particular the hip, which controls the position of the rest of the lower extremity, is very important. In the repetitive motion of walking, running or jumping the Achilles tendon is placed under tremendous load. In order to prepare the healing tendon to take this load, your physiotherapist will first prescribe ‘concentric’ muscle strengthening. Concentric contractions occur when the muscle shortens as it contracts. For example, when you rise up on your toes, your calf muscles are concentrically contracting and pulling on the Achilles tendon. Exercises such as calf raises will provide the appropriate stress to the tissues of the healing tendon to begin to prepare them for the forces of everyday activities. These exercises will first be done using both legs and when ready, we will progress you to doing them on one leg at a time in order to fully load the tendon with your body weight.
Eccentric contractions occur as the muscle lengthens and the tendon is put under stretch. Landing from a jump is an example of an eccentric contraction. As soon as appropriate, your physiotherapist will prescribe eccentric exercises for your Achilles injury. These contractions encourage the tendon to adapt to the more aggressive force that will eventually be needed to return to regular physical activity. Exercises such as raising up onto your toes on a step and then lowering down so that your heel is below the step is an eccentric calf exercise. Again, as appropriate, your physiotherapist will progress you to do this on just the injured side, and they will increase the speed of the lowering portion of the exercise to add even more force. They may also add weights to even further advance the force of the exercise. Repetitive jumping from a height and rebounding once you land is another advanced exercise that loads the tendon eccentrically. All exercises should be completed with minimal or no pain and advancing the exercises should be done at the discretion of your physiotherapist as not to flare up the healing tendon. Maintaining proper alignment of your entire lower extremity is paramount to decreasing the overall stress that is placed on your Achilles tendon so your physiotherapist will stress the use of proper technique and maintaining this alignment during all or your rehabilitation exercises.
In addition to strengthening and stretching, foot orthotics may be useful to correct your foot position, which in turn then encourages proper alignment up the lower extremity chain and decreases the stress on the Achilles tendon. Your physiotherapist can advise you on whether orthotics would be useful for you, and also on where to purchase them. We may try taping or strapping the bottom of the foot before encouraging you to purchase orthotics. This type of taping can give us a good indication if orthotics will be useful in decreasing your pain or changing your alignment before you actual purchase a permanent insert.
A critical part of our treatment for Achilles tendon problems at The Cambridge Physiotherapy includes education on returning to your full normal physical activity, whether that be a daily walking routine or a competitive level sport. The Achilles tendon takes stress during each step you take so an Achilles tendon that is recovering from injury can easily be aggravated. Returning to your normal physical activity at a graduated pace is crucial to avoid repetitive tendon pain or a chronic injury. Your physiotherapist at The Cambridge Physiotherapy will advise you on the acceptable level of activity at each stage of your rehabilitation process and assist you in returning to your activities as quickly but as safely as possible. With a well-planned rehabilitation program and adherence to suggested levels of rest and activity modification, most patients are able to return to their previous level of activity without recurring symptoms.
Tendonosis/Tendinopathy
If your Achilles problem is one of tendon tissue degeneration, healing and recovery may take longer and the injury will not respond to treatment designed to reduce inflammation. Two to three months or more of physiotherapy may be necessary. Correct treatment of tendonosis involves fostering new collagen tissue growth and improving the strength of the tendon.
Most importantly, a chronically injured tendon needs some relative rest while new collagen growth is encouraged. Limiting activities such as walking allows for a relative rest. Activities such as swimming or cycling can be substituted to allow a cardiovascular workout as long as they can be done in a fashion that doesn’t cause increased discomfort. Modalities for pain may also be used, such as ice or heat, but it should be remembered that their aim is to assist with local pain rather than inflammation. Your physiotherapist may use acupuncture or dry needling to encourage new collagen tissue growth of the chronically injured tendon. If available, your physiotherapist may also refer you to a doctor who performs injections of the blood to assist healing.
Autologous blood injections (ABI) and platelet-rich plasma injections are fairly new treatment techniques for chronic tendon problems and are still undergoing research regarding their efficacy. In ABI blood it taken from a patient and then injected right back into the injured tendon (under ultrasound guidance.) Platelet-rich plasma injections are similar but once the blood is withdrawn, only portions of the blood that are thought to be the most important for healing are injected into the tendon. These portions of the blood are highly active in creating new collagen growth of the tissues. (See Patient Guide Platelet-Rich Plasma Treatment.) Several injections may be done over a period of time depending on your doctor’s opinion and experience. A small rest period is usually encouraged while the tendon initially begins the healing process but then physiotherapy as described below is encouraged.
As your chronic tendon injury heals, your physiotherapist will prescribe similar stretching and strengthening exercises as described above under tendocalcaneal bursitis/paratendonitis. New collagen requires a controlled amount of stretching and strengthening to encourage the fibers to slowly adapt to the stresses of regular physical activity. If the appropriate controlled stress is not put through the tendon, a recurrence of symptoms will occur. Your physiotherapist at The Cambridge Physiotherapy will ensure you are not putting too much stress through your healing tendon, while also ensuring you can return to your regular activities as soon as possible.
Another form of therapy, called low-energy shock wave therapy, has been used successfully for chronic tendinopathy. This procedure causes high energy vibrations produced by the energy waves and is applied to areas of tenderness while the affected foot and ankle are gently moved in all directions. Shock wave therapy works by turning off nerves responsible for pain without affecting motor function. The procedure does not require anesthesia but it may take several treatment sessions before a difference is felt. This form of therapy also stimulates soft-tissue healing by increasing blood supply to the area treated. Newer treatments, such as blood and plasma-rich injections, as described above, are now more often being used rather than low-energy shock therapy.
Tendon Rupture
The success of nonsurgical treatment for an Achilles tendon rupture is under constant review. It is clear that treatment with a cast will allow the vast majority of tendon ruptures to heal, but it is not clear whether the incidence of re-rupture is significantly increased in those patients treated with casting for eight weeks when compared with those undergoing surgery. For this reasons many orthopedists still feel that Achilles tendon ruptures in younger active patients should be surgically repaired. Undergoing surgery, however, presents a wealth of other potential complications so the non-surgical treatment option, even with a potential for increased re-rupture, is currently being used as a viable treatment option for patients of all ages while ongoing research into the two treatment options occurs.
Non-surgical repair of an Achilles tendon rupture is often the recommended choice in all instances of the aging adult who has an inactive lifestyle. Nonsurgical treatment in this case allows the patient to heal while avoiding the potential complications of surgery. The patient’s foot and ankle are placed in a cast that holds the foot in a slightly pointed position for eight weeks. This position brings the torn ends of the Achilles tendon together and holds them until scar tissue joins the damaged ends. A large heel lift is worn in the shoe for another six to eight weeks after the cast is taken off. Rehabilitation at The Cambridge Physiotherapy begins once the surgeon feels it is appropriate. Aggressive rehabilitation is avoided as not to re-rupture the tendon or stretch it out too much. Your physiotherapist will closely liaise with your surgeon regarding the appropriate time frames for stretching and strengthening the injury. Similar rehabilitation principles as listed above in tendocalcaneal bursitis/paratendonitis section will be followed.
Surgery
Surgical treatment for inflammatory Achilles tendon problems is not usually necessary for most patients. Surgery options range from a tenotomy (a simple release of the tendon) to a more involved, open approach of repair.
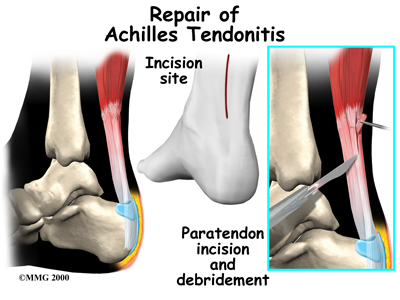 In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.
In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.
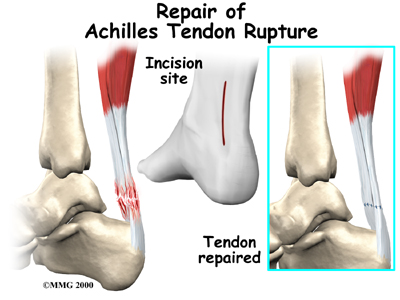
Surgery is also an option if you have a ruptured Achilles tendon. Reattaching the two ends of the tendon repairs the torn Achilles tendon. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. Numerous procedures have been developed to repair the tendon, but most involve sewing the two ends of the tendon together in some fashion. Some new repair techniques have been developed to minimize the size of the incision.
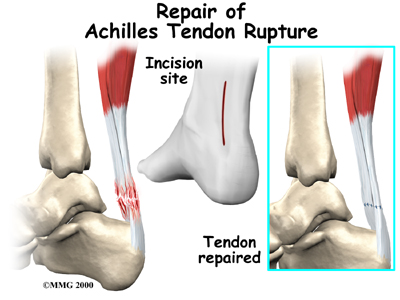
In the past, the complications of surgical repair of the Achilles tendon made surgeons think twice before suggesting surgery. The complications arose because the skin where the incision must be made is thin and has a poor blood supply. This can lead to an increased chance that the wound does not heal and infection sets in. Now that this is better recognized, the complication rate is lower and surgery is recommended more often. Usually, however, the patient will end up with a thickened tendon from the scar tissue surrounding the repair. This is considered normal, and generally has no effect, except aesthetically.
After Surgery
Traditionally, after a ruptured tendon has been repaired patients would be placed in a cast or brace for six to eight weeks after surgery to protect the repair and the skin incision. Crutches would be needed at first to keep from putting weight onto the foot. In the case of a debridement surgery, each surgeon will have his or her own post-operative protocol that you will need to follow regarding weight bearing and activity. This can vary significantly depending on your injury and the extent of debridement or repair completed while in surgery.
At The Cambridge Physiotherapy we highly recommend maintaining the rest of your body’s fitness with regular exercise even while you are in an immobilizer. Maintaining general cardiovascular fitness can be done with an upper extremity bike, as well as weights for the upper extremity and non-injured lower extremity. Upon removing the cast or brace, a shoe with a fairly high heel is recommended for up to eight more weeks, at which time physiotherapy begins.
In some cases, your surgeon may recommend physiotherapy much earlier than this. As immobilizing the leg in a cast can cause joint stiffness, muscle wasting (atrophy), and blood clots, patients instead wear a splint that can easily be removed to do exercises throughout the day. In this early-motion approach, physiotherapy starts within the first few days after surgery. The splint, however, continues to be worn while walking for six to eight weeks after surgery. When therapy is recommended early on, your physiotherapist may use electrical modalities such as ultrasound or interferential current to help decrease the pain and limit (but not prevent) post-surgical inflammation. Massage for the calf may also be helpful. Exercises in a pool may also be encouraged if you have a pool regularly available to you. The buoyancy of the water helps people walk and exercise safely without putting too much tension on the healing tendon. When physiotherapy is started early, the risk of aggravating the healing tendon, re-rupturing it, or over-stretching it is greater than when therapy is started after a more prolonged time of immobilization. For this reason, adhering to your physiotherapist’s advice regarding exercises and activity is crucial. Again, we will closely liaise with your surgeon to ensure you are advancing your rehabilitation as quickly as possible without risking further injury to your Achilles tendon.
As the tendon heals, more advanced stretching and strengthening exercises will be incorporated into your rehabilitation regime. Concentric and eccentric strengthening will be added as appropriate (see above.) If you are using a pool for your therapy, advanced exercises in the pool can also be added at this stage. An analysis of your alignment will also be done once you start moving more normally. Correcting any long-term alignment problems will avoid any aggravation of the tendon in the future.
As your symptoms ease and your strength improves, your physiotherapist will guide you through even further advanced stages of exercise. Athletes will begin running, cutting, and jumping drills by about the fourth month after surgery. Regular physiotherapy treatment usually ceases by approximately 4-5 months post surgery at which time your physiotherapist will only be used as a resource while you return to your normal activity. Athletes are usually able to get back to their sport by six full months after surgery. Remodeling of the tendon, however, can continue even up to 12 months post surgery. Usually rehabilitation after surgery for on your Achilles tendon progresses at The Cambridge Physiotherapy without any complications. If, however, during rehabilitation your pain continues longer than it should or therapy is not progressing as your physiotherapist at The Cambridge Physiotherapy would expect, we will ask you to follow-up with your surgeon to confirm that there are no complications such as delayed healing, infection, nerve damage, or scarring that are impeding your recovery.
Portions of this document copyright MMG, LLC.










 Where is the Achilles tendon, and what does it do?
Where is the Achilles tendon, and what does it do?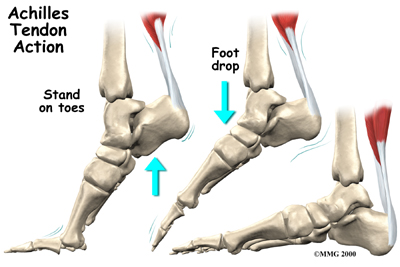
 A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.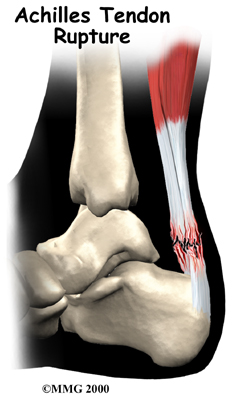
 It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.
It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.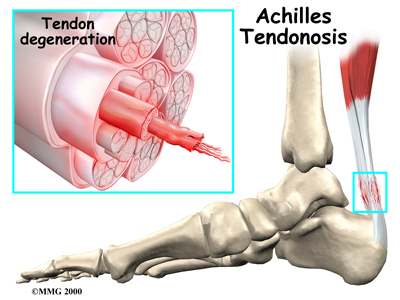 Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.
Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.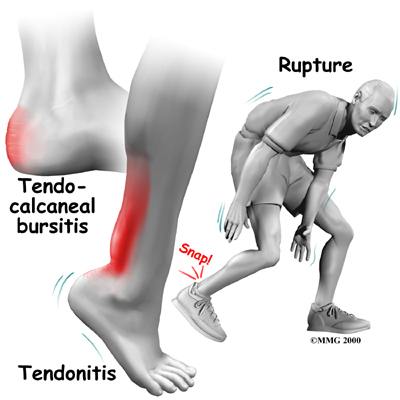
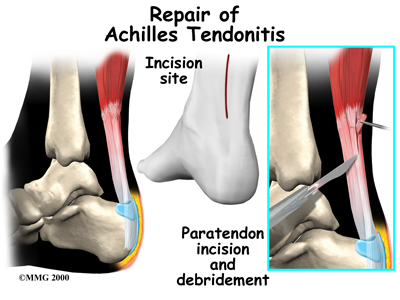 In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.
In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.