Introduction
Hand Physiotherapy in Cambridge, Galt, and Preston
Welcome to The Cambridge Physiotherapy's patient resource about Trigger Finger and Trigger Thumb.
Trigger finger and trigger thumb are conditions affecting the movement of the tendons as they bend the fingers or thumb toward the palm of the hand. This movement is called flexion.
This article will help you understand:
- how trigger finger and trigger thumb develop
- how doctors diagnose the condition
- what can be done for the problem
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hand Pain|limit:15|heading:Hear from some of our patients who we treated for *Hand Pain*#
Anatomy
Where does the condition develop?
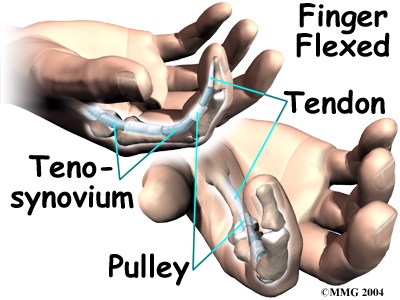
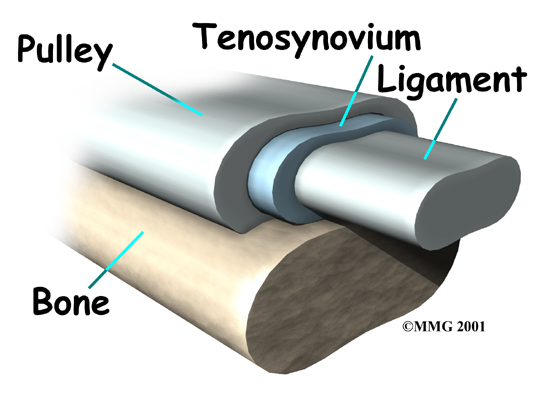
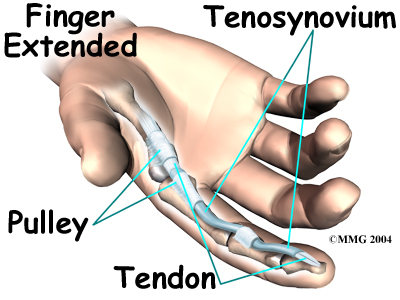
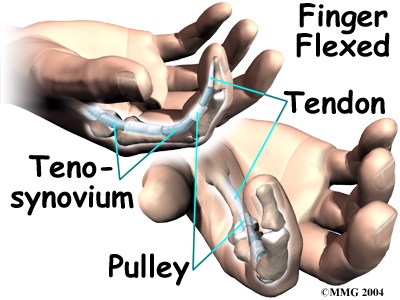
The tendons that move the fingers are held in place on the bones by a series of ligaments called .
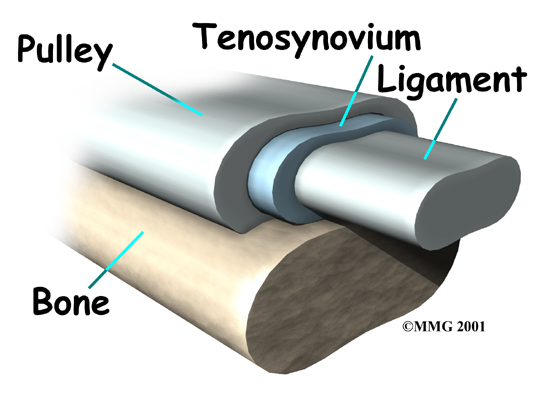
These ligaments form an arch on the surface of the bone that creates a sort of tunnel for the tendon to run in along the bone. To keep the tendons moving smoothly under the ligaments, the tendons are wrapped in a slippery coating called .
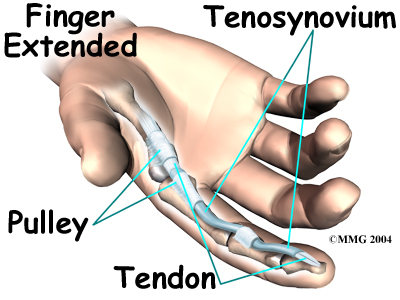
The tenosynovium reduces the friction and allows the flexor tendons to glide through the tunnel formed by the pulleys as the hand is used to .
Related Document: The Cambridge Physiotherapy's Guide to Hand Anatomy
Hand Anatomy Introduction
Causes
 Why do I have this problem?
Why do I have this problem?
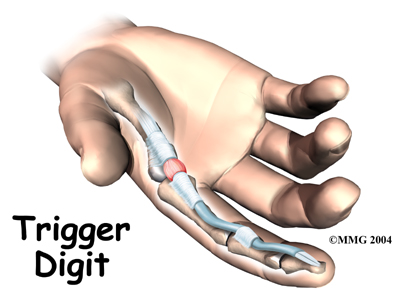
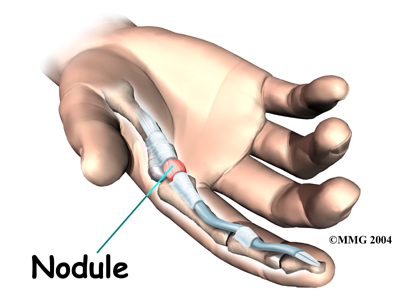
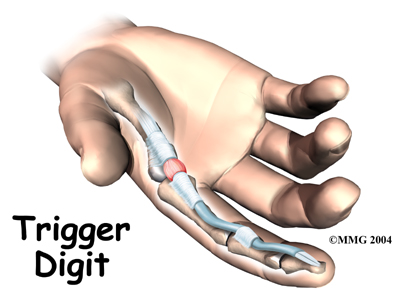
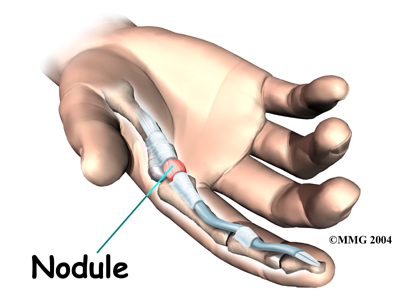
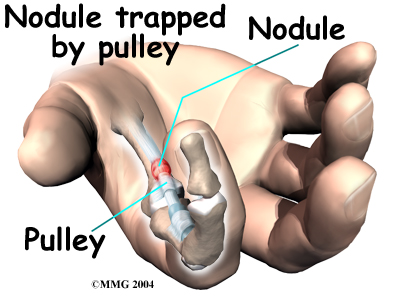
Triggering is usually the result of a thickening in the tendon that forms a , or knob. The pulley ligament may thicken as well. The constant irritation from the tendon repeatedly sliding through the pulley causes the tendon to swell in this area and create the nodule. Rheumatoid arthritis, partial tendon lacerations, repeated trauma from pistol-gripped power tools, or long hours grasping a steering wheel can cause triggering. Infection or damage to the synovium causes a rounded swelling (nodule) to form in the tendon.
Triggering can also be caused by a congenital defect that forms a nodule in the tendon. The condition is not usually noticeable until infants begin to use their hands.
Symptoms
What does a trigger finger or thumb feel like?
The symptoms of trigger finger or thumb include pain and a funny clicking sensation when the finger or thumb is bent. Pain usually occurs when the finger or thumb is bent and straightened. Tenderness usually occurs over the , at the bottom of the finger or thumb.
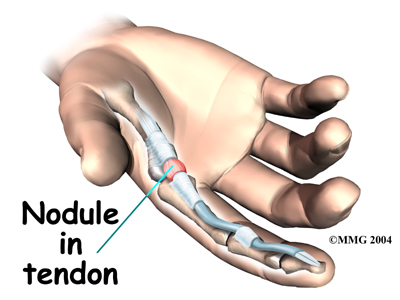
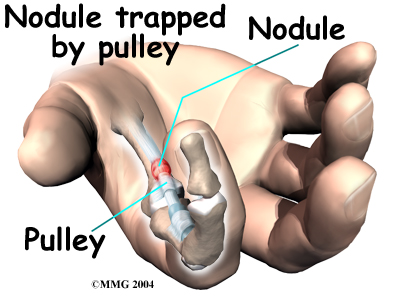
The clicking sensation occurs when the nodule moves through the tunnel formed by the pulley ligaments. With the finger straight, the nodule is at the far edge of the surrounding ligament. When the finger is flexed, the nodule passes under the ligament and causes the clicking sensation. If the nodule becomes too large it may pass under the ligament, but it gets stuck at the near edge. The nodule cannot move back through the tunnel, and the finger is locked in the .
Diagnosis
When you visit The Cambridge Physiotherapy, our physiotherapist will first take a history and do a physical exam. The diagnosis of trigger finger and thumb is usually quite obvious on physical examination. Usually a palpable click can be felt as the nodule snaps under the first finger pulley. If the condition is allowed to progress, the nodule may swell to the point where it gets caught and the finger is locked in a bent, or flexed, position.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at The Cambridge Physiotherapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
Non-surgical Rehabilitation
The Cambridge Physiotherapy programs of physiotherapy or occupational therapy are most effective when triggering has been present for less than four months. Our physiotherapists may build a splint to hold and rest the inflamed area. We will have you do special exercises to encourage normal gliding of the tendon. Your The Cambridge Physiotherapy physiotherapist will show you ways to change your activities to prevent triggering and to give the inflamed area a chance to heal. Our therapy sessions sometimes include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine to the sore area. This treatment is especially helpful for patients who can't tolerate injections.
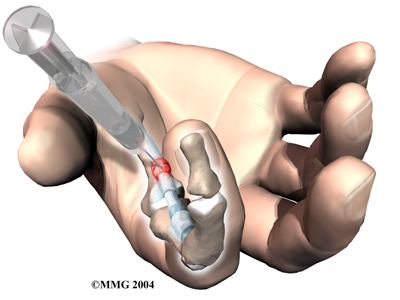
 Your doctor may recommend a into the tendon sheath to decrease the inflammation and shrink the nodule. This can help relieve the triggering, but the results may be short lived.
Your doctor may recommend a into the tendon sheath to decrease the inflammation and shrink the nodule. This can help relieve the triggering, but the results may be short lived.
When triggering has been present for more than four months, nonsurgical treatment is usually short-lived. You may get some relief of symptoms with a cortisone injection. If you wear a splint, the nodule may shrink temporarily, but patients often end up needing surgery for this problem.
Post-surgical Rehabilitation
You'll probably wear a fairly large padded bandage on your hand over the area after surgery until the stitches are removed. This is to provide gentle compression and reduce the bleeding and swelling that occurs immediately after surgery. The bandage can be removed fairly soon after surgery, aand is usually only required for the first 24 to 48 hours. When you begin your physiotherapy after surgery, we'll begin with gentle range-of-motion exercises.
You will particularly benefit from physiotherapy if your finger or thumb was locked for a while prior to surgery. In these cases, the finger or thumb may not straighten out right away after the surgery. Our physiotherapist may apply a special brace to get the finger or thumb to straighten it. We may also apply heat treatments, soft-tissue massage, and hands-on stretching to help with the range of motion.
Some of the exercises we’ll have you do are to help strengthen and stabilize the muscles and joints in the hand. Our physiotherapist will use other exercises to improve fine motor control and dexterity. We will provide tips on ways to do your activities while avoiding extra strain on the healing tendon. Although the time required for recovery varies among patients, as a general rule, you may need to participate in physiotherapy two to three sessions each week for up to six weeks.
At The Cambridge Physiotherapy, our goal is to help speed your recovery so that you can more quickly return to your everyday activities. When your recovery is well under way, regular visits to our office will end. Although we will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
The Cambridge Physiotherapy provides services for physiotherapy in Cambridge, Galt, and Preston.
Surgery
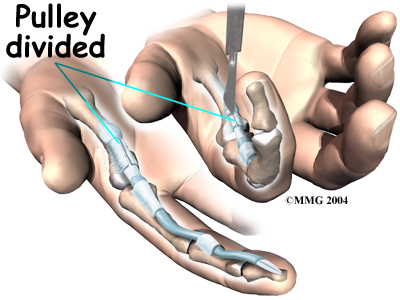
The usual solution for treating a trigger digit is surgery to open the pulley that is obstructing the nodule and keeping the tendon from sliding smoothly. This surgery can usually be done as an outpatient procedure, meaning you can leave the hospital the same day.
The surgery can be done using a general anesthetic (one that puts you to sleep) or a regional anesthetic. A regional anesthetic blocks the nerves going to only a portion of the body. Injection of medications similar to lidocaine are used to block the nerves for several hours. This type of anesthesia could be an axillary block (only the arm is asleep) or a wrist block (only the hand is asleep). The surgery can also be performed by simply injecting lidocaine around the area of the incision.
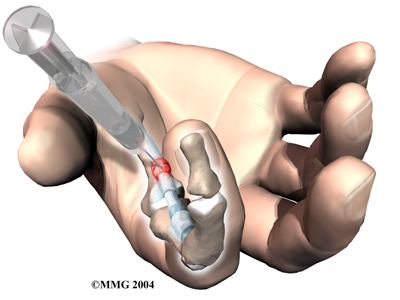
Once you have anesthesia, your surgeon will make sure the skin of your palm is free of infection by cleaning the skin with a germ-killing solution. An incision will be made in the skin. There are several types of incisions that can be made, but most are made along the natural creases and lines in the hand. This will help make the scar less noticeable once the hand is healed.
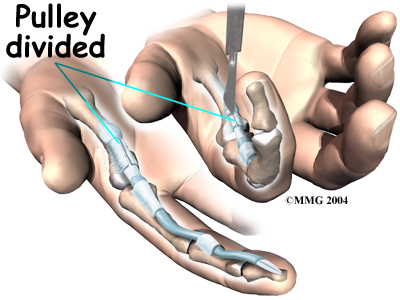
The skin and fascia are separated so the doctor can see the tendon pulley. Special care is taken not to damage the nearby nerves and blood vessels.
Next, your surgeon carefully divides the tendon pulley. Once the tendon pulley has been separated, the skin is sewn together with fine stitches.
Portions of this document copyright MMG, LLC.









 Why do I have this problem?
Why do I have this problem?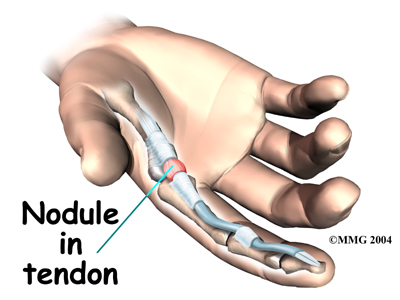
 Your doctor may recommend a
Your doctor may recommend a